
It seems the label “Medicare for All” is being attached to all sorts of proposals. Plans to provide universal healthcare coverage to Americans abound, but they aren’t all Medicare for All. Broadly speaking, “Medicare for All” applies to only those proposals that would cover everyone, replacing private insurance.
Other approaches are less drastic. For instance, some would give everyone the option to buy into government insurance (e.g., Medicare or Medicaid); if they preferred, they could continue to buy private insurance.
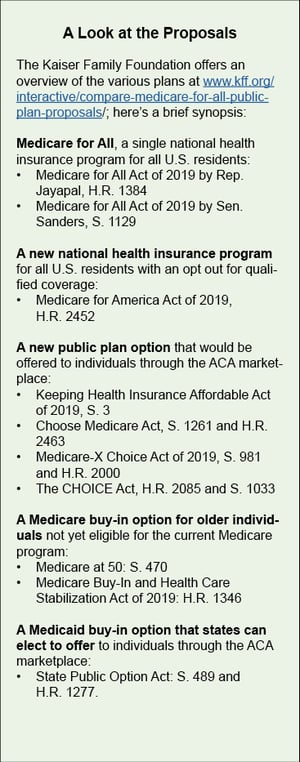
We’re going to focus on Medicare for All and the two pieces of legislation with the most traction:
- 1129, introduced by Sen. Bernie Sanders, calls for a single national health insurance program for all U.S. residents. The only out-of-pocket costs would be for some pharmaceuticals and certain elective procedures. It would be phased in over four years.
- The House bill introduced by Rep. Pramila Jayapal, H.R. 1384, would, in addition, cover long-term care. It has a two-year phase-in period. (For an overview of the various plans, see sidebar.)
What’s the potential impact on providers? Let’s start with hospitals.
How does Medicare for all affect Hospitals?
There’s no pat answer for how Medicare for All or similar proposals will affect hospitals, but a general picture is starting to emerge1.
Safety net hospitals: The impact on safety-net hospitals (and, for that matter, clinics) rests largely on how payment rates under the new plan compare to current Medicaid rates2. At first blush, it does appear that hospitals that treat a large number of uninsured patients would probably increase their revenue under the new system because they would no longer face the financial pressure of uncompensated care, Kaiser Health News explains3.
Hospitals serving the privately insured: In contrast, hospitals that treat many privately insured patients would likely see their revenues decline. That may not be a bad thing: Hospitals with significant influence or market power drive high costs because they can negotiate much higher rates with insurers, according to research published in Health Affairs.4
What about rural hospitals?
Medicare for All could strain already-beleaguered rural hospitals. If Medicare for All were to abolish private insurance and pay at Medicare levels, some hospitals--especially rural once--could close quickly with the drop in reimbursements, the New York Times reports5.
What do rural hospital leaders think? For the most part, they haven’t weighed in. “We’re so focused right now on keeping rural hospitals open and dealing with declining life expectancy that we haven’t engaged” with Medicare for All debates, Alan Morgan, CEO of the National Rural Health Association, told Kaiser Health News. He nevertheless offered some insights--and they are a bit less dire than the New York Times’ predictions.
Rural hospitals typically have tighter budgets, and lower government payments could be a strain, he acknowledges. But because rural hospitals often care for large numbers of uninsured patients, coverage expansions could be a plus. Moreover, special government programs and designations designed to keep rural hospitals afloat would likely continue unabated.
Getting paid through Medicare for all
Of course, we don’t know whether, under Medicare for All, providers--institutional and individual--would be paid at Medicare rates. Lawmakers could decide to match what they’re being paid now from both private and public insurers, Dr. David Blumenthal, a former Obama official and the president of the Commonwealth Fund, told the New York Times. “It would greatly reduce the opposition,” he said. “The general rule is the more you leave things alone, the easier it is.6”
If only for political reasons, it’s unlikely the government would pay all hospitals the current Medicare rates for all services7.
The two bills to provide a broad outline of how payments will be handled.
Jayapal’s H.R. 1384 proposal would pay institutional providers--hospitals, FQHCs, skilled nursing facilities, etc.-- based on a negotiated global budget. They would receive a lump sum payment for all operating expenses for covered services, both inpatient and outpatient. For individual providers, she calls for uniform fee schedules. Unlike the Sanders bill, it would establish a uniform national system for electronic billing for provider payments and a physician practice review board. These review boards would focus on quality, cost effectiveness and fair reimbursements for physician-delivered care8.
1129, the Sanders bill, includes less detail. It calls on HHS to establish a fee schedule “in a manner consistent with the processes for determining payments made under Medicare and establishes a new process for updating fees.”
At this point, the feasibility of Medicare for All remains in question. The mechanics? Details are scarce. And it’s far too soon to start taking bets on whether any sort of universal coverage, if any, will be enacted. Much depends on the 2020 election.
Where does Medicaid fit in?
As written, both Medicare for All bills would eliminate Medicaid. The role of Medicaid deserves more attention than it’s getting in the current debate, warns Drew Altman, president and CEO of the Kaiser Family Foundation, in a piece for Axios.9
For one thing, doing away with Medicaid would largely eliminate states’ role in the healthcare system. That could be a loss to all those who treat the underserved. Altman points out that state Medicaid programs are leaders in innovation--for instance, experimenting with delivery and payment reforms and addressing social determinants of health.
Meanwhile research continues to demonstrate the value of Medicaid. The latest study shows that expanded Medicaid coverage reduces mortality rates among low-income adults age 55-64--a group with relatively high mortality rates10. This July 2019 study from the National Bureau of Economic Research concluded as follows: “Our estimates suggest that approximately 15,600 deaths would have been averted had the ACA expansions been adopted nationwide.”
But what if Medicaid were the key to universal coverage? Medicaid for All isn’t a new idea, and legislation has already been introduced. An article in the Washington Post last year raised the idea that Medicaid provides a more nimble option if federal efforts stall11. A recent study published in the Ohio State Law Journal supports this notion, arguing that, under Medicaid statutes, states already have broad legal authority to expand access to the program as they see fit12. But that, of course, is just theory. We’re pretty sure that’s not going to happen in practice. But as we said, we’re not placing any bets.
Sources:
[1]“Delaney’s Debate Claim That ‘Medicare For All’ Will Shutter Hospitals Goes Overboard.” Kaiser Health NewsJune 2019
[2]Drew Altman, “Medicaid should be a bigger part of the ‘Medicare for All’ debate.”Axios, Jul 18, 2019
[3]“Delaney’s Debate Claim That ‘Medicare For All’ Will Shutter Hospitals Goes Overboard.” Kaiser Health NewsJune 2019
[4] Bai G, Anderson GF. “A More Detailed Understanding of Factors Associated with Hospital Profitability.” Health Aff (Millwood). 2016 May 1;35(5):889-97.
[5]https://www.nytimes.com/2019/04/21/health/medicare-for-all-hospitals.html
[6]https://www.nytimes.com/2019/04/21/health/medicare-for-all-hospitals.html
[7]“Delaney’s Debate Claim That ‘Medicare For All’ Will Shutter Hospitals Goes Overboard.” Kaiser Health NewsJune 2019
[8]https://www.healthaffairs.org/do/10.1377/hblog20170914.061996/full/
[9]Drew Altman, “Medicaid should be a bigger part of the ‘Medicare for All’ debate.”Axios, Jul 18, 2019
[10]Sarah Miller, Sean Altekruse, Norman Johnson and Laura R. Wherry. “Medicaid and Mortality: New Evidence from Linked Survey and Administrative Data.” NBER Working PaperNo. 26081.
[11]“The Health 202: 'Medicare for all' is the dream. 'Medicaid for more' could be the reality,” Washington Post, Aug. 2, 2018
[12]Wiley, Lindsay Freeman, “Medicaid for All?: State-Level Single-Payer Health Care” (July 30, 2018). 79 Ohio State Law Journal 843(2018); American University, WCL Research Paper No. 2019-03.: https://ssrn.com/abstract=3294046



